Violence against girls and women is often not included in discussions of women’s health; it is considered a social issue, not a medical issue.
1 in 5 women make their first disclosure of violence in an intimate relationship to their general practitioner.
So how do doctors ask their patient if she is experiencing violence from a partner? Especially since doctors are not trained to support women who experience violence in an intimate relationship. All doctors should receive training to recognize and respond to domestic violence.
One study of nearly 5,000 women, only 7 percent said a health professional had ever asked them about domestic or family violence. When surveyed, doctors often respond that they don’t ask such questions around intimate partner violence because of a lack of time, training and information on services that are available to help.
In April 2018, BWSS launched a campaign and resource kit designed to inform family physicians on how to respond to women be experiencing violence in their intimate relationships.
The Launch of the campaign resulted in UBC Medical School requesting training for their Family Practice Residents through annual seminars, beginning in 2019. On October 13, 2022, Angela Marie MacDougall, BWSS’ Executive Director, once again, presented on Intimate Partner Violence (IPV) and Partner Inflicted Brain Injuries (PIBI), to UBC Medical School family practice residents providing concrete information doctors can take when supporting patients who have experienced IPV and sharing the impacts of PIBI. By bridging the gap and giving general practitioners more information and resources in not only understanding the dynamics and impacts of IPV, but also how to have that conversation with their patients to ensure they receive the appropriate medical attention and personal supports.
Women who are abused often suffer injury to their head, neck, and face.
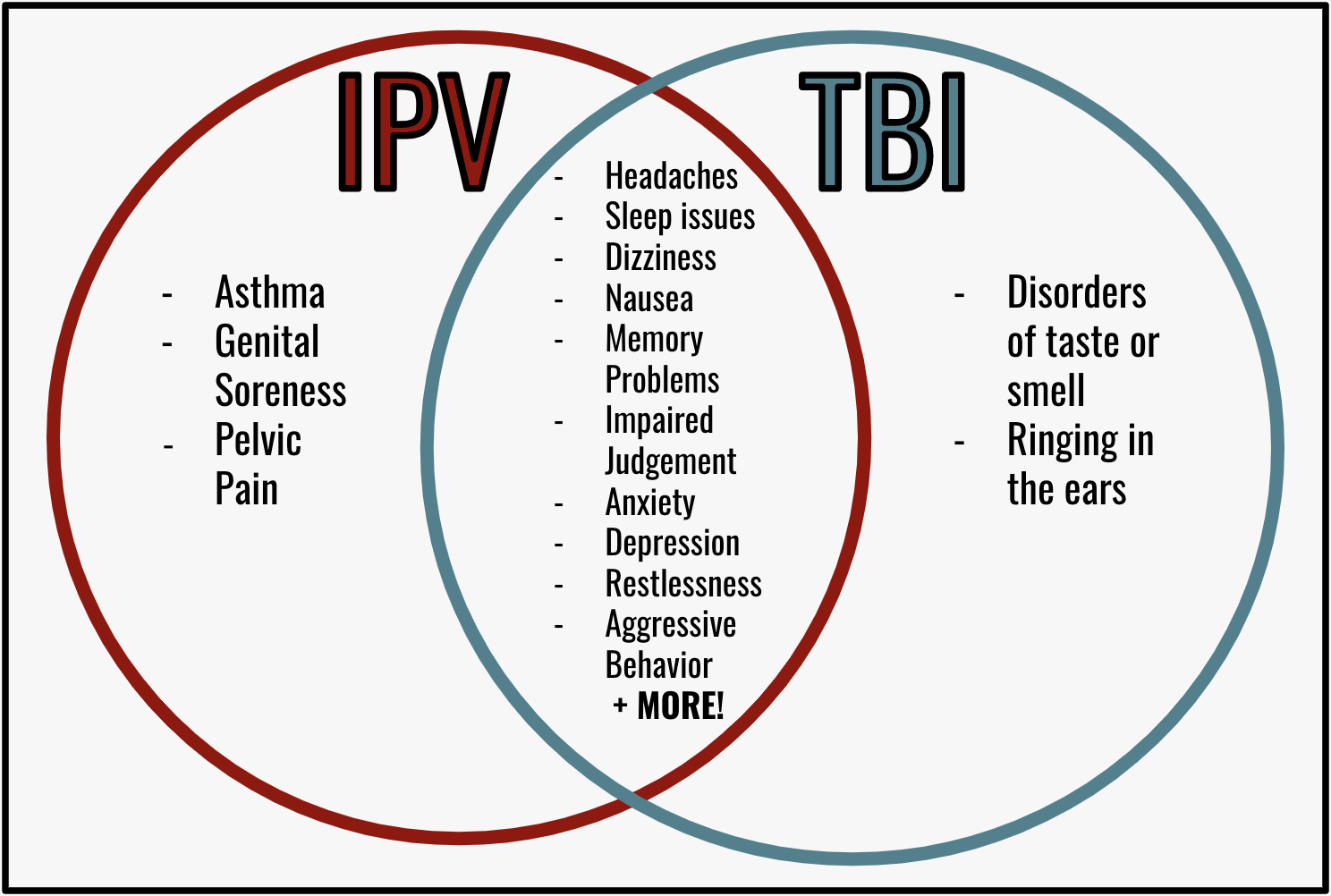
The high potential for women who are abused to have Partner Inflicted Brain Injuries that are mild to severe Traumatic Brain Injury (TBI) is a growing concern. The effects can cause irreversible psychological and physical harm. Strangulation can also cause TBI, because it prevents blood and oxygen from entering the brain leading to hypoxic injury, and sometimes anoxic injury.
One study found that 30% of battered women reported a loss of consciousness at least once and 67% reported residual problems that were potentially head-injury related.
When it comes to research around TBI the significant focus has been on male athletes and military personnel. Unfortunately, what is likely the largest group of repetitive TBI sufferers, namely women who experience intimate partner violence, has received scant attention.
Abusers who strangle are particularly dangerous. Strangulation is often a last escalation of terrible violence that precedes homicides . Victims who have been strangled are 7 times more likely to be killed by their partner. Strangulation is terrifying and traumatic. Over 70% of strangulation survivors believed they were going to die.
Many women are unaware they have experienced a traumatic brain injury because of the difficulty in diagnosing it since its symptoms often overlap with the impacts of intimate partner violence such as depression, anxiety, difficulty concentrating, etc.
It is so important that health care providers are aware of IPV and the link to TBIs, it could mean the difference between life or death for someone who is experiencing IPV.
Book training, workshops, or presentations for your organization here.